In the world of healthcare, lifestyle medicine is gaining momentum. Here, the focus is less about disease and more about taking control of health through lifestyle choices.

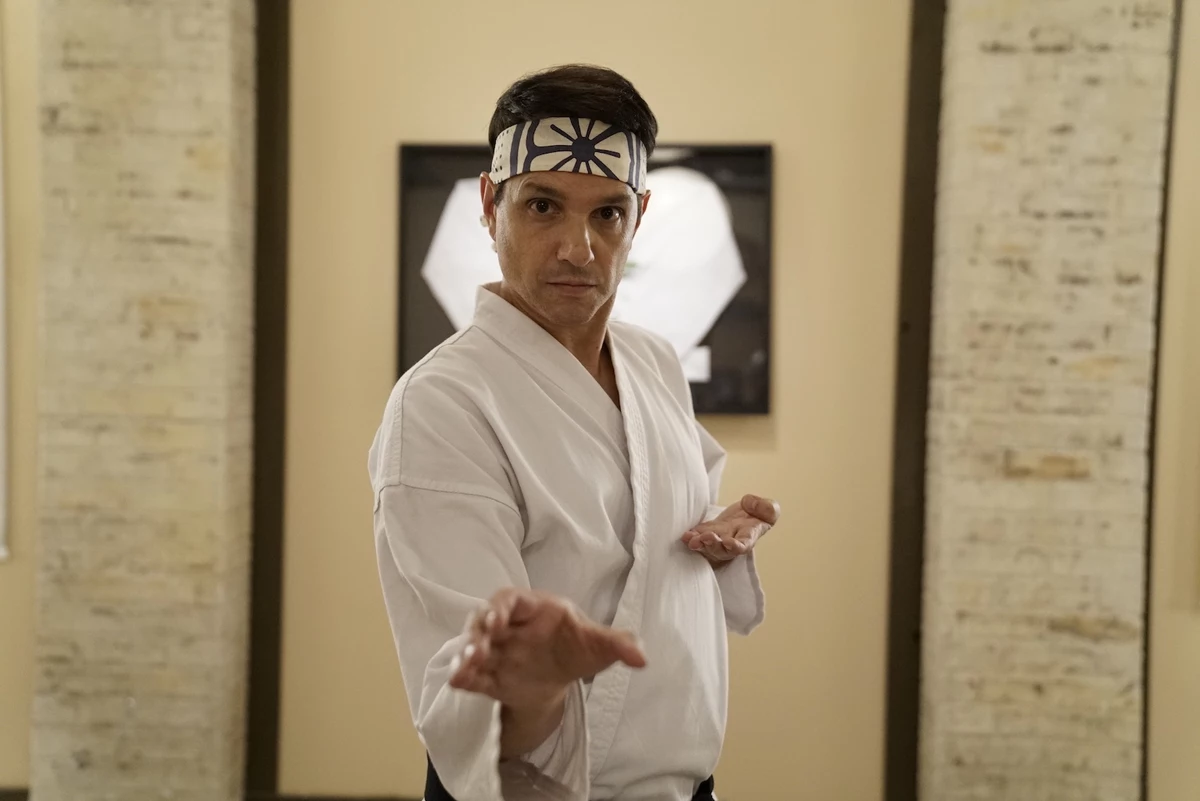
DR. IRIS GRANECK: Lifestyle medicine has ‘become a very big component of the preventive medicine training.’ Courtesy of Stony Brook Medicine
“Lifestyle medicine is a medical approach that uses evidence-based behavioral interventions to prevent, treat, manage and reverse chronic disease,” Dr. Iris Graneck, who chairs Stony Brook Medicine’s Department of Family, Population & Preventive Medicine. She spoke about the field on a webinar hosted by Stony Brook Medicine earlier in February.
Lifestyle medicine “is going to hopefully become part of all primary care specialties in the future because the current system of just treating chronic diseases is kind of a treadmill that is leading to more and more costs in medicine, and more and more diseases,” Dr. Raja Jaber, the medical director of Stony Brook Medicine’s lifestyle medicine programs, said on the webinar.
There are six pillars to lifestyle medicine. They include a whole-food, plant-predominant eating pattern; physical activity; restorative sleep; stress management; avoidance of risky substances; and positive social connections.
The area of lifestyle medicine is gaining traction at a time of an epidemic of chronic diseases that include diabetes, high blood pressure, obesity and more.
Lifestyle medicine has “become a very big component of the preventive medicine training,” Graneck said.
The specialty is taught at Stony Brook University’s Renaissance School of Medicine, Hofstra University’s Zucker School of Medicine and NYU Long Island School of Medicine.
By adopting the pillars of lifestyle medicine, it is possible to reverse many chronic diseases, leading to improved health, experts say. Even in medical practices that don’t have a dedicated lifestyle medicine practice, it’s not uncommon to find physicians who impart elements of lifestyle medicine to their patients.
It’s easy to see why, given the factors that lead to poor health.
“If we look at one of the biggest areas like risk for premature death or early death and … some of the contributors to that, and individual behaviors actually contributes 40% to the risk of early death,” Graneck said. “Social economic and environmental factors can contribute 20%, genetics 30%.”
These factors not only lead to poor health but are also costly to us as a nation.

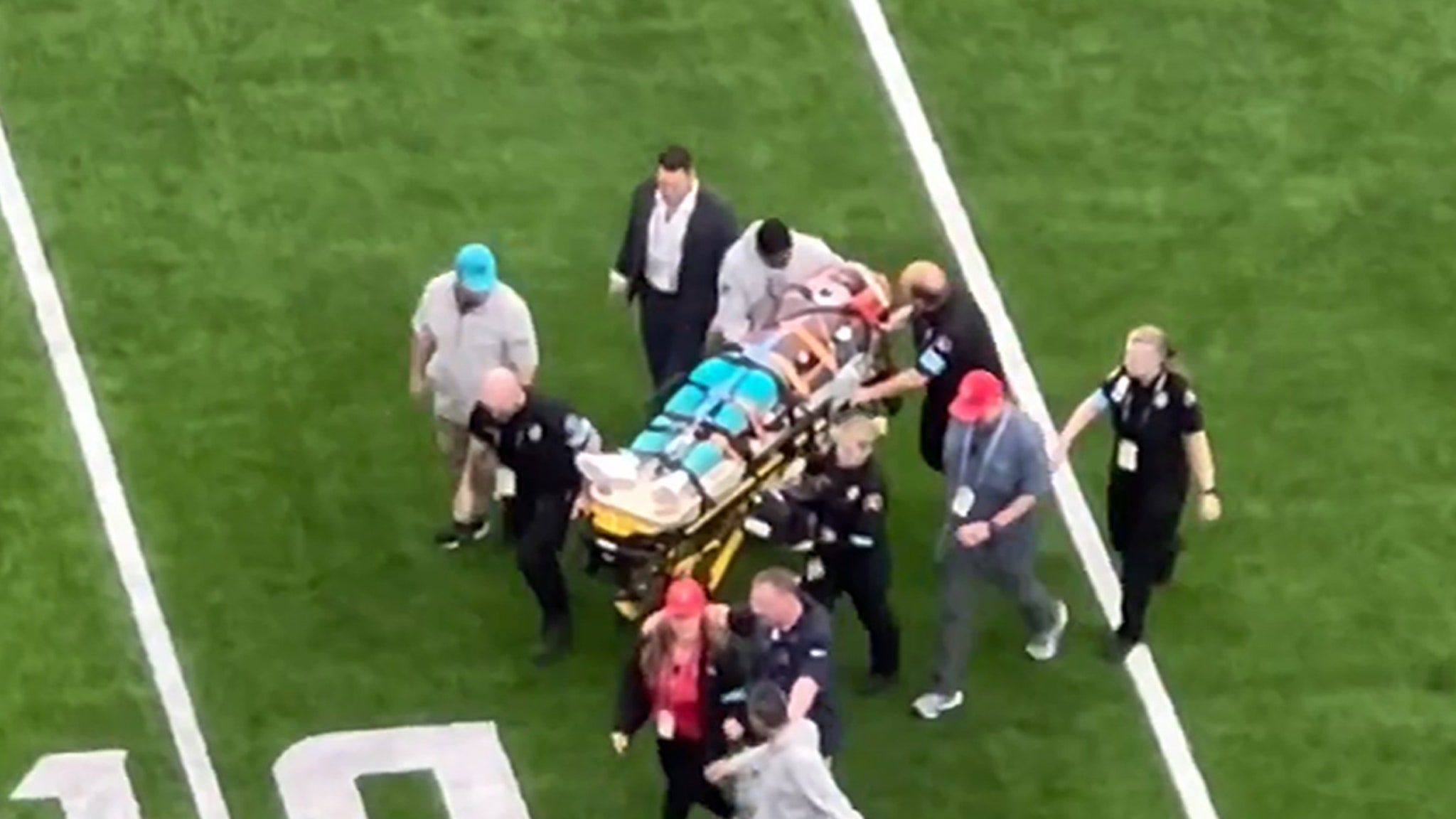
DR. RAJA JABER: ‘We can prevent up to 90% of diabetes, 80% of heart diseases and stroke and 40% of cancers.’ Courtesy of Stony Brook Medicine
Currently, “our general medical costs in the country are $4.1 trillion,” Jaber said. “That’s how much we spend on healthcare costs, and 90% of these healthcare costs go to treating chronic diseases.”
But by following the principles of lifestyle medicine – eating a mostly plant-based diet, exercising 150 minutes a week, sleeping well, connecting with others, and more – experts say populations become healthier.
“If we were to do that, then we can prevent up to 90% of diabetes, 80% of heart diseases and stroke and 40% of cancers,” Jaber said.
Lifestyle medicine got a big lift in December. That’s when New York City’s Mayor Eric Adams announced that the American College of Lifestyle Medicine in St. Louis, MO, is investing $44 million to provide every New York City healthcare practitioner free introductory training in nutrition and lifestyle medicine. The training is extended to hospitals in the city, including Northwell Health.
That focus is good news, especially regarding counseling patients on nutrition. According to PubMed.gov, 71% of U.S. medical schools do not reach the minimum benchmark of 25 hours of nutrition education set by the National Academy of Sciences.
But empowering people to eat more healthfully can lead to healthier populations.
“One of the most powerful aspects of lifestyle medicine is that patients become more engaged, active participants in their own self-care, disease prevention and management, and overall well-being,” Dr. Cindy Geyer, a board member of the American College of Lifestyle Medicine, said in a statement. “The end results include better health outcomes for patients and a fulfilling collaborative model of practice for physicians and other health practitioners.”
For example, according to PubMed.gov, lifestyle intervention reduced the incidence of Type 2 diabetes by 58%, compared with the drug Metformin, which reduced it by 31%.
True, the premise around the pillars may not seem revolutionary. Everyone knows they should eat well, exercise and get a good night’s sleep, for example. Yet, putting those concepts into practice can seem monumental.
That’s why the support of a lifestyle medicine practitioner “can be really powerful,” said Dr. Penny Stern, who 15 months ago began practicing lifestyle medicine at Northwell Health’s Center for Wellness and Integrative Medicine in Roslyn. There, new patients complete a “very thick intake form,” so Stern can hone in on the support they want.
“The importance of lifestyle behaviors on health is a cornerstone of primary care education,” said Dr. Gladys Ayala, professor of the Department of Medicine at NYU Long Island School of Medicine.
“Our curriculum not only teaches our learners about the importance of lifestyle factors on health; we also help students to acquire key communication skills that engender trust and understanding and that motivate patients to partner with us on their care,” Ayala said. “Motivational interviewing techniques are used to discuss diet, physical activity, tobacco use, alcohol use, illicit drug use, high risk sexual behavior, stress management, sleep hygiene, socialization, and medication adherence, to name a few.”
One could point to modern living as to how we’ve moved away from the pillars of health.
For example, “we’ve totally turned into a sedentary world,” Stern said. “We used to walk a lot, now we drive everywhere.”
In addition, people eat more processed foods in the United States than they did two decades ago. That consumption is linked to the higher risk of chronic disease, according to a 2021 study by NYU School of Global Public Health.

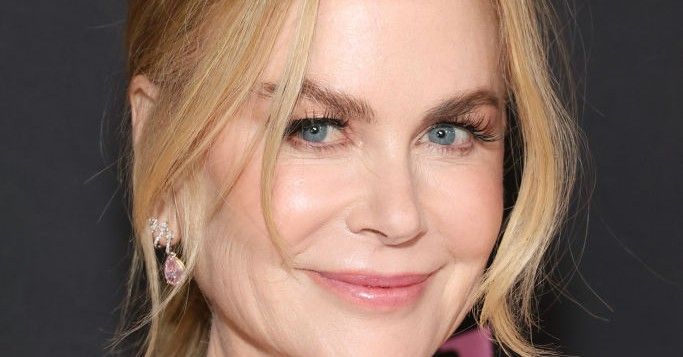
JOSEPHINE CONNOLLY-SCHOONEN: ‘Most people do know the basics of nutrition like broccoli is healthy and French fries aren’t healthy, but there’s so much food in the marketplace that is un-clear.’ Courtesy of Stony Brook Medicine
“Most people do know the basics of nutrition, like broccoli is healthy and French fries aren’t healthy, but there’s so much food in the marketplace that is unclear,” said Josephine Connolly-Schoonen, director of Stony Brook’s Medicine Nutrition Division, Department of Family, Population & Preventive Medicine, on the Stony Brook webinar. “A lot of foods are by big food industry, [which] created synthetic foods and are then marketed in a way that makes it very confusing for people to understand whether they’re contributing to health or not.”
Even our modern-day sleep habits have disrupted our health.
Prior to the invention of electrical light, “we went to sleep when it was dark, and got up when the sun rose – suddenly we are up till all hours. We run ourselves into the ground, watching TV or staying up to see the end of a movie,“ Stern said.
Stern tells patients to try an experiment – going to sleep when first feeling tired. “That’s when you’re meant to go to sleep.” Sleep is “the time when we rejuvenate and produce growth hormone, so you can restore, and repair,” she said. A poor night’s sleep leads to suppressed immune systems, accidents, poor relationships, low concentration and depression and other unfavorable outcomes, she said.
Social connections, too, are important to good health. When there is community, and a person doesn’t show up, others will reach out to find out why, Stern said. Even time spent with pets is beneficial. “People thrive when they have connections,” she said.
But, as Graneck pointed out, “changing behavior is not an easy thing.”
To offer support, Stony Brook Medicine offers a host of services and developed a lifestyle medicine website. The website includes information on each of the pillars and links to internal and external resources to specialists, coaches, programs, classes and more.

DR. PENNY STERN: Sleep is ‘the time when we rejuvenate and produce growth hormone, so you can restore, and repair.’ Courtesy of Northwell Health
Northwell’s Center for Wellness and Integrative Medicine also offers an abundance of resources including yoga, acupuncture, health and wellness coaching and other services. Where appropriate, Stern will refer patients to medical experts, including for nutrition counseling, or in the instances of sleep apnea to a sleep specialist, and others depending on the patient’s need.
Yes, there will always be a need for such experts as cardiologists, orthopedists and other specialists, but when it comes to helping people embrace the pillars of health, lifestyle medicine “can be so transformative,” Stern said.
By adopting these pillars, “we can prolong our life by 10 years,” Jaber said.
People can have “not only a longer life, but free of disease, and that’s what we want. We don’t want to have a longer life where we are in and out of hospitals or in a nursing home. We want to live and live very healthily.”
[email protected]



























































![OG Boo Dirty Fet Finesse2Tymes – “Unappreciated” [Official Music Video] OG Boo Dirty Fet Finesse2Tymes – “Unappreciated” [Official Music Video]](https://i.ytimg.com/vi/uaEFrPJHASg/maxresdefault.jpg)